By Nicolas Gambardella
We are all familiar with the words ‘blood clots’, ‘stroke’ and ‘heart attack’. However, before the media deluge devoted to the extremely rare side effects of certain COVID-19 vaccines, few outside the medical community had heard of thromboembolic events.
The central player in the drama is the thrombus, also known as blood clot. The blood clot is the product of coagulation. The formation of a clot stops a haemorrhage when the blood vessel wall is damaged. The first step is forming a platelet plug formed by the aggregation of platelets, or thrombocytes. The thrombus is then consolidated by strands of fibrin.
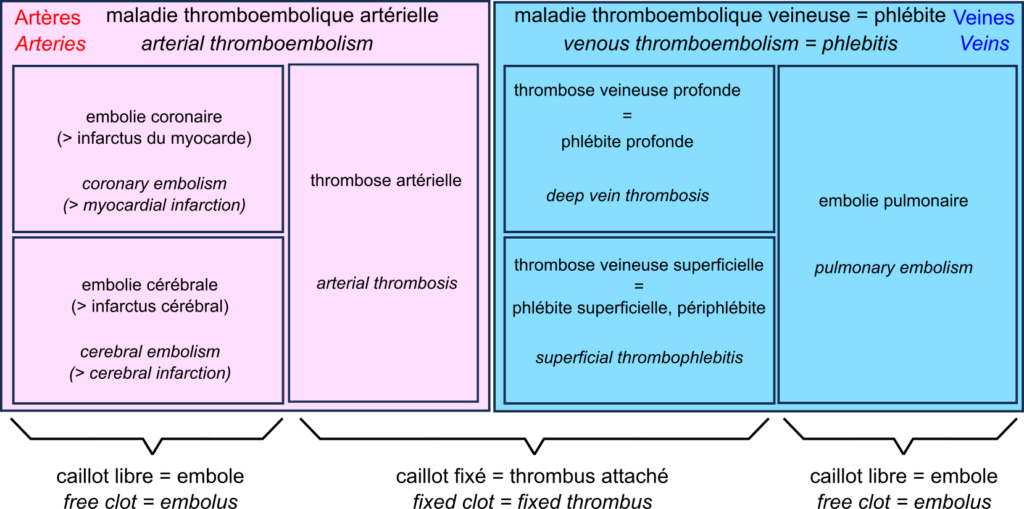
A thrombus can block vessels, especially if they are already narrowed, for example in atherosclerosis. This thrombosis impedes blood flow. Thrombosis occurs mainly when the blood flow is slow and steady (otherwise, the clots are torn off). This is why they are primarily found in the veins, forming deep vein thrombosis, also called deep phlebitis, or superficial thrombophlebitis.
A thrombus can break off, forming an embolus that travels through the vessels following the blood flow. If the vessels become smaller, the embolus is more likely to block them. Such an embolism decreases the blood supply downstream, depriving the tissues of oxygen, something called ischaemia, leading to tissue necrosis or infarction.
In the veins, oxygen-deprived blood flows from the small vessels to the large vessels. Therefore, if a clot breaks loose, it does not block the downstream vessels and travels to the heart. It is then sent by the heart into the pulmonary artery. This artery, in turn, splits into smaller and smaller branches, and the clot can then block the circulation. This is a pulmonary embolism. Deep vein thrombosis and pulmonary embolism are two manifestations of venous thromboembolism or phlebitis.
In the arteries, blood flow is rapid and pulsating. As a result, arterial thrombosis is quite rare. However, as the circulation moves from large to small vessels, embolisms are common. The most common examples are coronary artery embolisms, causing destruction of the heart muscle, a myocardial infarction, and cerebral artery embolisms causing cerebral infarction, one of two types of stroke – the other being cerebral haemorrhage.
This brings us to a very rare complication of COVID-19 vaccination with adenovirus vector vaccines such as Vaxzevria from Oxford University and AstraZeneca, and Ad26.COV2.S from Janssen. This complication is called “vaccine-induced prothrombotic immune thrombocytopenia (VITP)”. Indeed, in extremely rare cases, these vaccines induce antibodies to recognise the protein “platelet factor 4“, which activates platelets and causes their aggregation, leading to thrombosis.
Let’s reiterate that these cases are extremely rare, and their incidence is much lower than that observed after infection with SARS-CoV-2, thromboembolic events being one of the main complications of COVID-19.