By Nicolas Gambardella
Covid-19 affects all of us on a daily basis and discussions about the disease stir passions, whether among politicians, health professionals, scientists, or the general public. Commentary and debate, particularly about the seriousness of the pandemic and how to counter it, are often tainted by inaccuracy and even bad faith due to confusion between different concepts and misunderstanding of some of them. People talk about different things, compare things that are not comparable, and misrepresent what others are saying.
I’m not a doctor or an epidemiologist. My opinions are my own, and I am certainly not in a position to provide advice. This post is not intended to take a position, but to provide some clarity on concepts that have been thrown around in pieces of news and in raging tweets.
Are Covid-19 and SARS-CoV-2 the same thing?
No, Covid-19 and SARS-CoV-2 are not two names for the same thing. Covid-19 is a “disease“, which is a set of symptoms related to an identified common cause (as opposed to a “syndrome“, which is a set of symptoms with an unknown, uncertain, or irrelevant cause). This disease is due to the infection of humans with the SARS-CoV-2 virus. This infection is the cause of the disease, not the disease itself. A large part of the population shows no symptoms after SARS-Cov-2 infection, people are said to be “asymptomatic”. In other words, these people are not sick. According to studies, this population is estimated to be between one-third of those infected to several times the number of people having the disease.
So we can see that there is a big difference in seriousness depending on whether we’re talking about the virus infection or the disease. SARS-CoV-2 infection is generally not very serious compared, for example, to Ebola or rabies viral infections. On the other hand, because of the severe respiratory symptoms and the lack of treatment, Covid-19 disease is actually more dangerous than rabies.
The disease is diagnosed on the basis of symptoms, before hospitalization, during hospitalization, or post-mortem. Only a certain proportion of patients are tested for the presence of the virus. It is generally accepted that for all patients with symptoms of Covid-19 and positive for the virus, the virus is the triggering factor for the disease. But it must be remembered that we are all permanently infected with several viruses (sometimes several strains of the same virus). For patients who are not tested for the presence of the virus, the decision depends on local policies. Hence, for example, the debates on the very low mortality from Covid-19 in Russia, or the real extent of deaths in care homes.
To summarise, not all persons infected with SARS-CoV-2 are sick with Covid-19, and it is possible that in a small proportion of persons diagnosed as sick with Covid-19 (especially in post-mortem diagnoses) the disease was in fact not triggered by SARS-CoV-2.
Above, I used the word “mortality”. So it’s time for a little vocabulary check.
Mortality, Lethality, Case Fatality Rate, Infection Fatality Rate
The “mortality” of a disease is the number of people killed by that disease in a given population, including those without the disease. The “lethality” of a disease is the number of people killed by the disease in patients with the disease. The lethality of a disease does not depend on its “prevalence“, while this is the case with mortality. In most countries, seasonal flu has a much higher mortality rate than Ebola hemorrhagic fever, although the latter has a much higher case fatality rate.
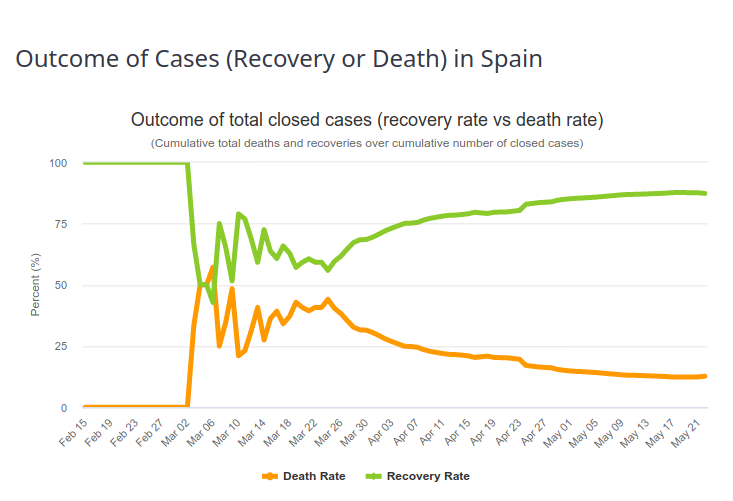
In order to estimate the fatality rate of a given infectious disease, the observed values of deaths in the sick population must be matched. The observed value is the Case Fatality Ratio (CFR). The estimated value is the Infection Fatality Ratio (IFR). One would think that with a well-constructed and careful assessment these numbers are close. They are not. The first reason is described in the previous paragraph (the difference between infection detection and disease diagnosis). The second is that the case-fatality rate changes over time. The first patients diagnosed usually have severe forms, with high mortality. The observed case-fatality rate is therefore very high (an extreme case being 100% if the first patient dies). As the diagnosis is extended to a larger population, and as the management of patients improves, the proportion of people surviving the disease increases. And the case-fatality rate tends to the infection fatality rate i.e., the “true” case fatality rate. This evolution can be seen in the image below, representing the outcome of Covid-19 diseases in Spain (Source https://www.worldometers.info/coronavirus/country/spain/, 23 May 2020). The first patient recovered, and then for a period of time 50% of the patients died, which corresponds approximately to the fraction of deaths of Covid-19 patients on ventilators. Then, the recovery rate increases more or less steadily.
It is very important to understand that if 10% of the patients diagnosed with Covid-19 in a given area and at a given time die from the disease, it absolutely does not mean that 10% of the people infected with the virus will die from it.
Can lethality be compared between countries? Influence of testing policies
In order to assess infection-fatality rates, it is, of course, necessary to measure case fatality rates and to be able to detect cases. There are two types of tests.
So-called serological tests detect the presence of antibodies in the blood that target the virus. These tests can tell if a person has been infected in the past. There are two main problems with these tests. First, at the moment we do not know exactly what proportion of infected people create antibodies. In the case of infected people who have developed Covid-19, it seems that the amount of antibodies is related to the severity of symptoms (probably because symptoms are related to the amount of virus, the “viral load“). The big unknown is for people who have not developed the disease. Second, these tests are generally not very reliable, and in particular, their “sensitivity” is not high enough (more details in this post).
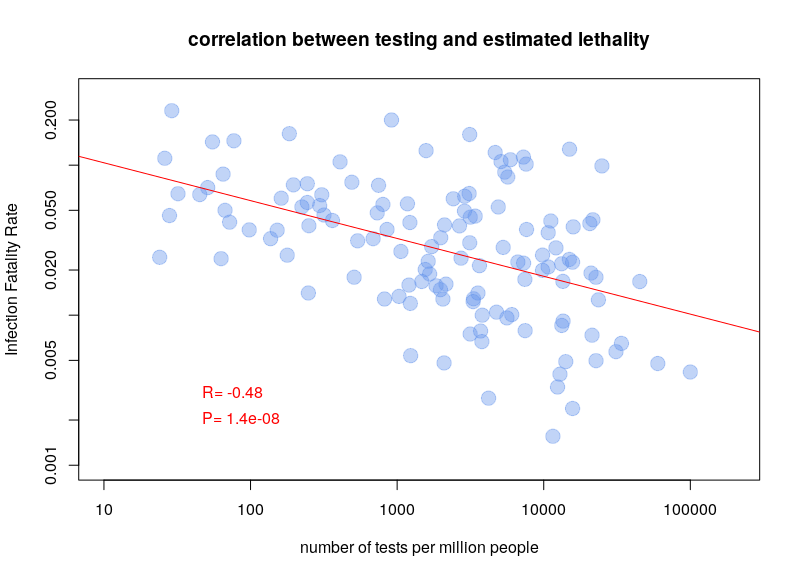
The other type of test detects the presence of the virus in actively infected people. The problem with these tests is that they have to be repeated over and over again. For a few days after infection, the viral load is not sufficient to be detected. Also, after a few weeks, the virus is no longer detectable. A person who had symptoms of Covid-19 can now be negative. Nevertheless, this is the type of test used to calculate case fatality rates. It is therefore clear that the testing policy will influence the calculations. If a country only tests people entering the hospital, the case fatality rate will be higher than if a country tests the whole population. It is therefore not surprising that there is a very clear correlation between case-fatality rates and the number of tests performed per million inhabitants. The graph below is based on Worldometer data from 10 April 2020.
Can lethality be compared between countries? Influence of age structure
Different studies have attempted to calculate an overall lethality rate of Covid-19 for the whole population, see for example here, here, and here. These estimates are based on data obtained by different methods (e.g. disease diagnosis, virus detection, detection of antibodies to the virus) in disparate regions, and analysed in a variety of ways. Not surprisingly, the results are, to say the least, heterogeneous. What they have in common is the desire to determine a “universal” rate. Trying to determine a single lethality for a disease is a justifiable exercise. However, this rate can only be valid for a homogeneous population and will necessarily vary between populations, making comparisons difficult, if not irrelevant.
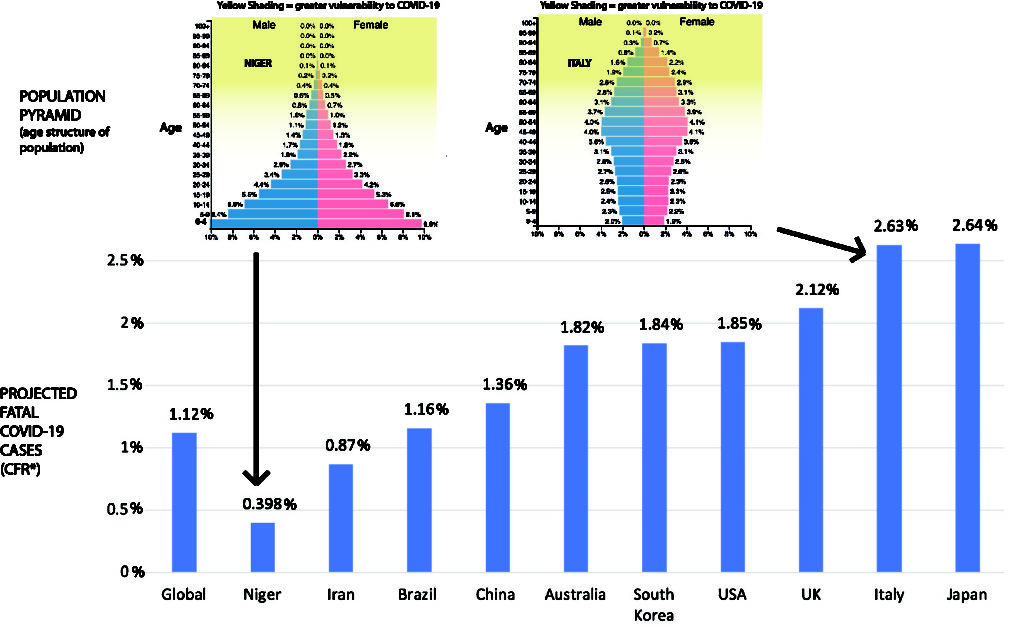
The first factor is the effect of age. Most respiratory diseases disproportionately affect the elderly. As a result, infections with the viruses that trigger these diseases, such as influenza, show highly age-dependent mortality. Similarly, an estimate of the lethality rate of Covid-19 in China was 0.0016% for children aged 0-9 years and gradually increased to 7.8% for those over 80 years of age, an increase of almost 5,000 times.
If lethality depends on age, so does mortality. However, the relationship is not direct because of the distribution of the population by age group (the population pyramid). There are many more people aged 60 to 85 than there are aged 85 to 110. Although Covid-19 is much more lethal in the latter population, there are more deaths in the former. Since different countries have different age pyramids, this will affect their overall estimated lethality, as shown in the figure below (borrowed from https://theconversation.com/the-coronavirus-looks-less-deadly-than-first-reported-but-its-definitely-not-just-a-flu-133526)
However, beware, things are not that simple. As the UN showed as early as 1955, the global mortality curve is affected by life expectancy. Mortality at age 25 in a country with a life expectancy of 60 is similar to mortality at age 45 in a country with a life expectancy of 70. This is due to the underlying causes of lower life expectancy. Which brings us to the comorbidities.
Can lethality be compared between countries? Influence of comorbidities
Stricto-sensu, comorbidities are the other disorders that will affect the outcome of the disease. However, for this post, I mean all the factors not related to SARS-CoV-2 infection that will affect the lethality of Covid-19. One research paper studied many of these factors in a large cohort of over 96,000 patients from six continents (the purpose of the study was to study the effect of drugs on Covid-19, but that is not our point here). If each year of life increases the risk of Covid-19 death by 1%, one BMI point increases it by 6%, having diabetes by 20%, smoking by 27% and being Hispanic by 50%! These different factors are of course not independent (and therefore not additive).
The impact of ethnicity may come in part from genetic predisposing factors, as well as environmental conditions. For example, it is clear that the transmission of SARS-CoV-2 is affected by temperature and humidity as well as air pollution. It is not impossible that the outcome of the disease may also be affected (possibly via respiratory co-morbidities).
Finally, the state of health systems has a considerable impact on the number of Covid-19 deaths. While most patients have only mild symptoms (let alone asymptomatic people), a fraction of patients requires respiratory assistance. In the worst case, these people need to be intubated. A large fraction of these people survive. In health care systems with insufficient ventilator capacity, all of these patients die. This is regardless of the policies undertaken to contain or eradicate the disease. However, these policies are important to keep the number of patients with severe Covid-19 below the limits of the health care system (“flattening the curve”).
Herd immunity collective or lockdown policies
One of the inexhaustible sources of sterile and acrimonious debate is the battle between advocates of “herd immunity” and those of “isolation”. The latter notion is familiar to everyone and fairly simple to understand. If people are isolated, through social distancing and confinement, they cannot be contaminated or contaminate others. Moreover, if we quarantine the sick long enough for them to recover and get rid of the virus, we can eradicate it. Obviously, in the case of SARS-CoV-2, the goal is no longer to eradicate it, as the number of infected people is too large and their geographical distribution too wide. The aim is to reduce the number of severe diseases as much as possible while waiting for a vaccine.
Herd immunity means that a sufficient portion of the population is exposed to the virus and develops an immune response so that the chance of an unexposed person encountering an infected person is very low. For many viruses, the required proportion of the population is just over 80%. Note that this principle of herd immunity is a key aspect of vaccination campaigns. In order for a campaign to keep disease at bay, a certain portion of the population must be vaccinated. Building up such herd immunity also goes hand in hand with isolating vulnerable people until the required % of immunized people are reached (no one suggests, as is sometimes written, that the herd immunity strategy means sacrificing a % of the population corresponding to the IFR, i.e. almost 1% of the world’s population).
Estimates of the % of the population that has developed immunity to SARS-CoV-2 infection vary between 1% and 25% depending on the study. A cohort study in Geneva observed a growth rate of 3% per week. This percentage is obviously far from sufficient for a society to rely on herd immunity. Does this mean that the idea of herd immunity is invalidated? Not at all. At best, it reflects the success of isolation policies. In the long term, the consequences of isolation policies might outweigh the consequences of SARS-CoV-2 infection, especially if effective vaccination or treatments, whether curative or prophylactic, are not forthcoming.
The important thing is that the two approaches are incompatible and therefore the consequences of the application of one cannot be used to judge the other. Moreover, between absolute quarantine and uncontrolled exposure, there is a continuum of possibility. For example, an interesting approach, based on the fact that Covid-19 is mainly severe in elderly subjects or those with co-morbidities, is the concept controlled avalanche based on voluntary infections.
Of course, this post only deals with some of the concepts underpinning the heated debates about Covid-19. However, I hope you will use it as a starting point to explore the diversity of opinions available and avoid the pitfall of snap judgements. Everyone is in the same boat and is looking for the same thing: a resolution to this crisis with the fewest possible casualties and consequences.